 This page explains the indications for, process of an induction of labour, and the risks associated with induction. The information will also be discussed with you to help you make an informed decision about your care and aims to answer frequently asked questions. If you require any further information, please ask a Midwife or a Doctor.
This page explains the indications for, process of an induction of labour, and the risks associated with induction. The information will also be discussed with you to help you make an informed decision about your care and aims to answer frequently asked questions. If you require any further information, please ask a Midwife or a Doctor.
This information will use the term ‘woman’ throughout. This should be taken to include people who do not identify as women, but who are pregnant or have given birth.
What is Induction of Labour?
In most pregnancies, labour starts naturally between 37 and 42 weeks leading to the birth of the baby but in some cases labour will be started artificially. This is called induction of labour.
Every woman’s pregnancy and labour is different therefore, it is important that we plan your care together taking into consideration the individual needs of you and your baby. You need to balance the risks of continuing your pregnancy versus the risks of being induced to decide if induction of labour is right for you.
The Doctor or Midwife will discuss all of your options with you (and any support person you wish to bring to the appointments) and the risks and benefits of induction in detail. They will also discuss with you, all of the alternatives to induction.
They will support you to make informed decisions concerning your care. They will also support you to make a plan of care going forward if you do not wish to have your labour induced. You can also change your mind, decide to await spontaneous labour or discuss alternative options at any time during the process.
This information, which is based on current national guidance, will explain the:
- Reasons induction of labour may be offered.
- Process and methods of an induction of labour.
- Risks associated with induction.
The information will also be discussed with you to help you make an informed decision about your care and aims to answer frequently asked questions. If you require any further information, please ask a Midwife or a Doctor.
Why am I being offered induction of labour?
The decision to offer an induction of labour will be based on current national guidance. About 1 in 3 women will have their labour induced.
The most common reasons are:
- You have reached 41 weeks gestation.
- Your membranes (waters) have broken spontaneously, but labour has not started.
- You have a medical condition, for example, diabetes or pre-eclampsia.
- You are expecting twins.
- Your baby is smaller or bigger than expected for your current gestation.
- Your baby has a medical condition.
- Your baby’s movements are reduced.
If you are being offered induction of labour for a medical problem, such as diabetes or high blood pressure, the Doctor will explain your individual risks to you or your baby’s health.
Induction of labour will be discussed with you from 38 weeks of pregnancy to give you time to consider this information and make a choice. At your 40 week appointment and an offer made to arrange an appointment to have your labour induced if this is your decision.
If your pregnancy is 41 weeks or more, the risks to you and your baby may increase. The chance of your baby developing health problems increases and it is known that in some cases the placenta may not function as well after this time. The table below looks at outcomes for babies and mothers who birthed based on gestation.
|
Potential outcome: |
41 weeks |
42 weeks |
|
Caesarean birth |
326 in 2836 (11.5%) |
344 in 2834 (12.13%) |
|
Admission to neonatal intensive care |
85 in 2834 (3%) |
123 in 2827 (4.35%) |
|
Stillbirth / Neonatal death |
1 in 2835 (0.04%) |
10 in 2834 (0.35%) |
Induction of labour from 41+0 may reduce these risks but may impact your birth experience. See outcomes for women that are likely to be the same with induction at 41 weeks and 42 weeks:
- Maternal death.
- Caesarean birth.
- Meconium aspiration syndrome.
- Hypoxic ischemic encephalopathy (HIE).
- Assisted vaginal birth (e.g. forceps or ventouse).
- Unassisted vaginal birth.
If the offer of induction is because your baby’s weight is estimated to be above the 95th percentile, at or after 36 weeks, the risks and benefits of induction or awaiting spontaneous natural labour are:
|
Potential outcome: |
Induction of labour |
Awaiting spontaneous natural labour |
|
Shoulder dystocia |
41 per 1000 |
68 per 1000 |
|
Third or fourth degree tear |
26 per 1000 |
6.9 per 1000 |
Outcomes for babies and women that are likely to be the same with induction of labour and awaiting spontaneous natural labour:
- Perinatal death.
- Caesarean birth.
- Brachial plexus injury to baby (an injury to the nerves that run between the neck and the shoulder).
Reduced Fetal Movements are a reduction in or change to your baby’s normal pattern of movements. See NHS Your baby's movements page for more information.
If you are being offered induction of labour because of RFM, you need to take into consideration the following information, before making your decision:
One episode of RFM at or after 39 weeks - Data suggests that a single episode of RFM increases the risk of stillbirth is doubled (from 1 in 813 to 2 in 813).
Recurrent episodes of RFM (which is defined as two or more episodes within a 21 day period after 26 weeks gestation) - Data suggests that recurrent RFM increases the risk of stillbirth 5 times more likely (from 1 in 813 to 5 in 813).
Because of the data above, there is the potential that your baby’s reserves for labour may be reduced if RFM occurs recurrently or beyond 39 weeks. This means they may not cope as well with the labour. As scans and fetal heart monitoring cannot definitively tell us your baby will cope with labour, we offer options for you to choose regarding how your baby is monitored in labour. Fetal Monitoring in Labour leaflet.
On the Midwifery Led Unit, Intelligent Intermittent Auscultation (IIA) using a hand held device can be used to your baby’s fetal wellbeing. This is a safe method for pregnancies where the baby is at low risk of fetal distress.
On the Labour Ward Suite, IIA can also be carried out but an alternative is continuous electronic fetal monitoring (CEFM). CEFM is used to monitor your baby’s wellbeing more closely in those at higher risk of fetal distress. CEFM is recommended by NICE if there are RFM within 24 hours of the onset of labour.
The detection of and acting upon fetal distress may take longer when using IIA in comparison to CEFM. This is because slight/subtle changes will be more quickly identified when monitoring continually. In extreme cases, this delay could result in a higher chance of a poor outcome for babies.
Prior to starting the induction process, you may wish to consider approaches that may lead to your labour starting spontaneously.
There have been many methods suggested over the years that have been said to start labour, but the truth is we don’t really know what starts labour. Some methods are unsafe so do not try anything until you have read the information below.
Prior to starting the induction process, you may wish to consider approaches that may lead to your labour starting spontaneously.
Aromatherapy
This is for women planning to give birth on the Midwifery Led Unit, with no underlying health conditions. The blend of oils used helps to relax the body, which in turn may increase your oxytocin levels, and encourage the uterus to start contractions.
Appointments last for up to 30 minutes and involve an aromatherapy treatment such as a footbath or massage and the offer of a membrane sweep. We also provide a small amount of the essential oil blend for you to use at home.
Your Community Midwife will talk to you towards the end of your pregnancy about when it is suitable for you to attend the aromatherapy clinic.
Appointments are made via Antenatal Clinic Reception on 01270 612478.
Membrane Sweep
A membrane sweep can be offered at antenatal appointments. It has been shown to increase the chances of labour starting naturally within the next 48 hours (after the sweep) and can reduce the need for other methods of induction of labour.
Membrane sweeping involves your Midwife or Doctor carrying out a vaginal examination, where they will ‘sweep’ their finger in a circular motion around the neck of your womb (cervix) to separate the membranes from the cervix. It can be carried out at home, during an outpatient appointment, or in hospital. It works better if the cervix is slightly favourable (opening and softening).
You might experience pain, discomfort, a small amount of blood loss or a mucousy blood stained show from the procedure, but it will not cause any harm to your baby. Some women choose to wear a sanitary pad or panty liner to the appointment. It is your decision whether you choose to have a membrane sweep. If you are concerned about the amount of bleeding you should contact Maternity Triage.
You may choose to have additional membrane sweeping if labour doesn’t start spontaneously after the first sweep. Your Midwife will plan your appointment for this with you.
We understand the importance of meeting your birth preferences. We will discuss these with you and endeavour to meet them. We will plan your care together to ensure you understand how the options available may affect your preferences.
If you are considering a homebirth please discuss an alternative place of birth or alternatives to induction of labour with your Midwife.
Vaginal examinations are required as part of the induction process to ensure we can offer the most appropriate care pathway.
Labour pain can start quickly. Contractions can be more intense and closer together than they are in a labour which starts naturally, therefore you may require additional pain relief.
Your choice of how you would like your baby’s heartbeat to be monitored may need to be reconsidered as induction of labour can make contractions start suddenly and frequently which can reduce your baby’s oxygen supply. Continuous monitoring may be offered.
If you require an oxytocin infusion your baby may become distressed due to the strength and frequency of contractions, therefore this is only safe to do so with continuous fetal monitoring.
Continuous fetal monitoring cannot be carried out on the Midwifery Led Unit therefore you would be offered birth on the Labour Ward.
We will make an initial assessment, including a vaginal examination, which will let us know the most appropriate method of induction. This is based on the Bishops Score which will give you a score out of 10. This looks at softness, position, length, how open your cervix is and how deep your baby’s head is in the pelvis. We will discuss this with you and consider the most appropriate method of induction.
There are 4 options for medical induction offered by the Trust, which are outlined below. One or more may be suitable for your circumstances.
Propess® pessary
Propess®) Pessary is not a suitable method of induction for everyone. There are some contraindications (circumstances where it should not be used). These can be found in the following leaflet at www.
Some examples are previous caesarean birth or previous surgery on the womb due the potential risk for uterine rupture. It also not suitable for patients who have had unexplained vaginal bleeding during pregnancy. Your Doctor or Midwife will discuss this with you and offer an alternative if Propess® is not suitable for you.
 The hormone pessary (Propess®) is small, flat rectangular shaped pessary which looks a little like a tampon. It is inserted into the vagina, behind the cervix, and contains the hormone dinoprostone which stimulates cervical ripening (softening) and the onset of labour. Propess® can remain in the vagina for up to 24 hours. It will be removed prior to this if:
The hormone pessary (Propess®) is small, flat rectangular shaped pessary which looks a little like a tampon. It is inserted into the vagina, behind the cervix, and contains the hormone dinoprostone which stimulates cervical ripening (softening) and the onset of labour. Propess® can remain in the vagina for up to 24 hours. It will be removed prior to this if:
- Labour becomes established (when you are having regular contractions every 3 minutes).
- Your waters break spontaneously.
- You are having too many contractions or they are lasting too long.
- You are experiencing any side effects such as nausea, vomiting, low blood pressure or increased heart rate.
- Your baby is showing signs of distress.
 The Propess® pessary is inserted during a vaginal examination; This may be slightly uncomfortable but should not be painful. Depending on the Bishops Score, the pessary will be inserted. You will be asked to lie down for 20-30 minutes afterwards. The pessary will absorb the moisture from your vagina which makes it swell like a tampon) and settle into place. This reduces the chance of it falling out. You will need to take care when:
The Propess® pessary is inserted during a vaginal examination; This may be slightly uncomfortable but should not be painful. Depending on the Bishops Score, the pessary will be inserted. You will be asked to lie down for 20-30 minutes afterwards. The pessary will absorb the moisture from your vagina which makes it swell like a tampon) and settle into place. This reduces the chance of it falling out. You will need to take care when:
- Wiping yourself after going to the toilet.
- After washing.
Image Source: www.
You may be able to go home after it is inserted. See Outpatient Induction of Labour Section.
Once the Propess® pessary has been inserted, we would actively encourage you to mobilise. If you are remaining in the induction bay and not going home, you are welcome to leave the Labour Ward Suite. However, you must stay within the hospital grounds. Please inform a member of staff before you leave the ward.
The Propess® pessary will be removed when your labour has become established (when you are having regular contractions). Once labour is established you will be transferred to either the Labour Ward or Midwifery Led Unit.
Propess® works differently for every woman therefore we are unable to confirm how long it will be until you are in established labour.
It is not unusual for the Propess® pessary to fall out. This quite often occurs when you go to the toilet or if your waters have broken. Please check the toilet prior to flushing in case it has fallen out.
If the Propess® falls out, please inform a member of staff as it can be replaced quite easily.
If labour has not yet started after 24 hours the Propess® will be removed, you will be transferred to the Labour Ward when a bed is available to continue with the induction process. This may be by Artificial Rupture of Membranes and/or Oxytocin Infusion. On occasions, due to the unpredictable nature of the workload on the unit, transfer may not be immediate. We apologise for the inconvenience this may cause but please be assured that the safety of you, your baby and the other women on the unit are our priority. All information and explanations will be given to you if this situation occurs.
Are there any risks to induction with Propess®?
The risks associated with induction of labour with Propess® are:
- Hyperstimulation (contractions lasting for more than 30 seconds that come every two minutes or lasting more than 2 minutes).
- Labour may be more painful once it starts.
- The induction of labour may be unsuccessful.
- You may need to birth your baby with the assistance of instruments such as forceps or ventouse.
Are there any side effects?
The hormone pessary can occasionally produce some side effects which are usually mild and include: nausea, vomiting, dizziness, palpitations and fever. If you experience any of these you must let the Midwife know.
For more information about Propess® see the medicines information leaflet www.
Cervical Ripening Balloon
This is an option if you have had a previous caesarean birth or prefer this method to Propess®. This is inserted by the Doctor or Midwife during a vaginal examination.
A Cook® Balloon Catheter is a silicone tube which has two inflatable balloons. Sometimes we may need to put your legs in stirrups to insert the balloon catheter. A speculum is inserted into the vagina and the cervix is cleaned with water. The catheter is inserted through the cervix and the balloons are inflated carefully with fluid so pressure is applied to the cervix. This softens and dilates the cervix so that your waters can then be broken. The speculum is removed and the catheter is loosely taped to the thigh or supported in a second pair of underwear.
The two balloons then adapt to the contour of the cervical canal to minimise discomfort. When the catheter is removed, the cervix will be assessed for dilatation (opening of the cervix) and based on the findings (Bishops Score) a plan will be made with you regarding the next stage of the induction of labour. The Cook® Cervical Ripening Balloon is made to naturally and gradually dilate the cervix and help start labour. Ripening and dilation works by the balloons’ gentle and constant pressure from both the internal and external cervical canal. This allows pressure from the two balloons to ripen the cervix.
As the Balloon does not contain any medication, it reduces the risk of side effects. Once inserted into the vagina the Cook® Balloon will usually stay there for approximately 12 hours. It can be easily removed should it need to be taken out before this time.


The balloon will be removed after 12 hours, an assessment made and plan of care discussed with you based on the finding. This will either be Propess®, artificial rupture of membranes or a caesarean birth if artificial rupture of membranes is not possible.
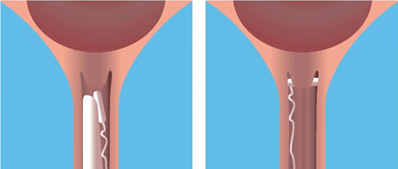
Artificial Rupture of Membranes (ARM)
This is when the membranes (waters) around your baby are artificially broken during an internal vaginal examination. This will cause no harm to your baby, but the vaginal examination needed to perform this procedure may cause you some discomfort. Breaking your waters is done with a small plastic hook during a vaginal examination.
Oxytocin Infusion
Oxytocin occurs naturally in the body and in labour causes the uterus to contract. An infusion of artificial oxytocin via a drip may be used to stimulate contractions and start labour. Once contractions have begun, the rate of the drip can be adjusted so that the contractions occur regularly until your baby is born. You will need to have the baby’s heartbeat monitored throughout the labour, but you will still be encouraged to mobilise and remain in upright positions. You can still use the birthing pool as waterproof, wireless monitoring is available on the Labour Ward.
Inductions are commenced at different times throughout the day. A time will have been arranged for you to arrive at the Induction Suite.
There is a possibility that if the maternity unit is very busy it may be necessary to change your allocated time. This is to ensure that you and your baby receive a safe service. We will explain everything to you and keep you informed of any further changes.
When you arrive at hospital for your induction, you and your birthing partner will be welcomed into one of four individually partitioned rooms. These rooms are called the ‘Induction Suite’ and are directly linked to the Labour Ward.
Each room has a television and there are kitchen facilities available to make yourself drinks and a snack. You will be shown around the ward to familiarise yourself with the setting.
The wellbeing of you and your baby will be monitored throughout the process; however, you will not receive one to one care during your stay in the induction area.
You may be able to go home once the induction process has been started if it is safe for you to do so (see Outpatient Induction).
What happens before my labour is induced?
Before starting the induction process, a Midwife will carry out an antenatal assessment to assess you and baby’s wellbeing. This will include taking your observations, checking what position your baby is laying in, and a monitoring of your baby’s heart rate. In this time, the Midwife will again discuss with you the reasons why induction has been offered, the process of induction, and answer any questions you may have.
If you and your baby’s observations are normal, and you wish to proceed, the Midwife will ask you for your consent to carry out a vaginal examination to assess which method of induction is most suitable.
Visitors
Due to the limited space available and enhanced security measures we are pleased to welcome one support person, at a time, in the Induction area. There is no visiting in the Induction area for any other friends or family members.
One support person may stay with you overnight. However, it is important to remember that your labour may not establish for a number of hours so your birthing partner may provide better support if they are well rested at home. Your birthing partner will be contacted once your labour is established and you require support.
A second birthing partner is welcome to join you once your labour has become established and you have been transferred to Labour Ward. Two birthing partners may be with you during labour.
Meals
Meals are provided for all women who are being induced. A self-service breakfast is always available in the kitchen and a cooked meal at lunchtime and sandwiches in the evening will also be provided. Women who are being induced also have access to a small kitchen where they are welcome to make themselves a drink of tea and coffee throughout their stay. Your birth partner is welcome to bring their own snacks or use the hospital shop or café.
The menu may be limited for those with dietary requirements, you may wish to bring your own food with you. Please note there are no facilities for reheating meals.
Is there anything I can do to help labour start once induction has begun?
You can continue with your day to day activities and eat and drink as normal.
You can help to increase the natural oxytocin levels in your body by hand massaging and expressing colostrum from your breasts, which will help support and enhance your induction and may help your labour to progress quicker.
Oxytocin also helps stimulate breastmilk production, the first milk you make is called colostrum. This is essential for your baby’s immune system and protects against infection from birth.
If no colostrum is produced, don’t worry, this is often the case, massage and hand expression will increase your oxytocin levels. This helps contract your uterus to contract, which then helps to stimulate your milk supply, ready to give your baby straight after birth, if you wish. Ask your Midwife to show you how to hand massage and express. She will show you where to store any colostrum you have collected.
Remember, induction of labour is usually a long process, often taking more than 24 hours. This is normal, try to stay calm and do something that will help the time pass more quickly.
It is very important you have a supportive birthing partner with you. Choose someone who has a positive attitude about birth and who you feel totally relaxed, confident and comfortable with.
What to do while you are waiting for regular contractions to start:
- Take a leisurely walk and keep mobile.
- Watch television or films (something that makes you laugh is best).
- Take a warm bath or shower.
- If contractions are irregular, slow down or stop, have a short nap or a lie down.
- Do some relaxation techniques.
- Keep your breathing quiet and sigh out slowly during contractions.
- Ask your birth partner to give you a massage.
- Use your TENS machine if you plan to use one.
- Put a heat source, wrapped in a small towel on areas that ache.
- Keep upright and mobile.
- Change your position frequently.
- Try a birthing ball – do circular movements whilst sitting on the ball.
- Drink plenty of fluids.
- Eat little and often – carbohydrates like bread or pasta and sugary foods are best.
It is best to try and stay as relaxed as you can.
When do I need to alert a Midwife?
- Contractions / Abdominal pain.
- Fresh red vaginal bleeding.
- Backache.
- Your waters have broken.
- New symptoms.
- You have difficulty in passing urine.
- Concerns about your baby’s movements.
- You require pain relief.
- You have pain in an abdominal scar area.
- You are worried.
For cervical ripening balloon
- The balloon catheter falls out.
- You have difficulty in passing urine.
You may also wish to have a discussion about:
- Your plan of care.
- Concerns you or your partner may have.
- What happens next.
What happens if induction does not work for me?
Sometimes induction of labour is not successful and your labour does not start. If this is the case alternative methods or a caesarean birth will be offered to you.
Outpatient induction of labour means you start the process of induction of labour in hospital and you may be able to go home following an individual assessment.
Why have outpatient induction of labour?
An outpatient induction of labour:
- Reduces the amount of time you will need to stay in hospital before your labour begins.
- It can involve fewer vaginal examinations.
- Enables you to spend more time in your home environment with your family.
- Makes the process of induction feel less medical.
Who can have outpatient induction of labour?
- Your pregnancy is between 37 - 41 weeks gestation.
- Your pregnancy is uncomplicated.
- You have a singleton pregnancy.
- Your BMI is less than or equal to 40.
- Your age is less than or equal to 40 years.
- You have diet controlled gestational diabetes.
- Your baby has been identified as possibly being large on scan.
- You have not had a previous precipitate labour (<2 hours).
You must also:
- Have a good understanding of written and verbal information given to you.
- Have an adult remain with you.
- Not be reliant on public transport.
- To be able to attend the hospital within 30 minutes.
- Have a functional telephone/mobile.
- Be confident to go home.
The Doctor or Midwife will discuss the option of outpatient induction with you and you can change your mind either way during the process e.g. you can go home if you had chosen to stay or return to the hospital if you are at home.
Please remember to bring your hand-held notes with you and an overnight bag just in case you need to stay in hospital.
The Propess® will be inserted and when the Midwife is happy with your observations and if you are happy to, you can go home to wait for signs that labour has started.
A Midwife will call you 6-12 hours after you have gone home to check how you are doing and to see if you have any concerns. If this call is due out of hours, a Midwife will call you first thing in the morning. If you need any advice or reassurance, you can call Maternity Triage on 01270 273116.
You will be given a date and time to return to the induction suite.
What happens when I go home?
The pessary works by ‘ripening’ your cervix – this means the cervix softens, shortens and begins to open up. You will commonly feel a period-like ache while this happens, but sometimes stronger contractions occur and labour may start. In the very early stages of labour contractions can vary in length and how often they come. They may continue for several hours but not become much longer and stronger. This is normal. It is OK to stay at home during this time until you are in labour.
When your contractions change, they become longer, stronger and closer together and usually continue to become stronger until the baby is born. If you experience signs of labour and are not sure please don’t hesitate to call the hospital for advice.
You should contact Maternity Triage immediately for advice on 01270 273116 if you experience any of the following:
- If you start having regular contractions.
- If you think your waters have broken (this may be a gush of fluid or a continual dribble of fluid from your vagina).
- If you are concerned about your baby’s movements, such as reduced or altered fetal movements.
- If you have continual abdominal pain.
- If you have vaginal swelling or soreness.
- If you feel unwell, have difficulty breathing, have vomiting or diarrhoea.
- If you start bleeding vaginally.
- If your Propess® pessary falls out.
- If you at all worried or have any questions
What happens when my contractions are regular?
You should ring the Maternity Triage on 01270 273116 when your contractions become regular. You will be advised to return to the hospital for monitoring of your baby’s heartbeat. If you have planned a homebirth you will be asked to attend the hospital for monitoring of your baby’s heartbeat and if this is normal you may return home to birth your baby.
24 hours have passed what should I do now?
You will be given a time to return to hospital to continue the induction process, if you wish to do so.
The Propess® pessary will be removed. You will be transferred to the Labour Ward when a bed is available to have your waters artificially broken and a hormone drip may be commenced if required.
On occasions, due to the unpredictable nature of the workload on the unit, transfer may be delayed. We apologise for the inconvenience this may cause but please be assured that the safety of you, your baby and the other women on the unit are our priority. All information and explanations will be given to you if this situation occurs.
Please see artificial rupture of membranes and oxytocin section of 'how will my labour be induced' in this leaflet for more information.
Before making your decision we advise you to ask yourself the following questions:
- Why am I being offered induction and why now?
- What pain relief options will be available to me?
- What will be the effect for my baby?
- What steps above are specifically being offered to me?
- What is the impact on my place of birth?
If you are unsure or have further questions, please speak to Midwife or Doctor who can explain further.
You may also wish to consider using the decision making aid 'BRAINS'.
Benefits: Reduces the risks associated with continuing your pregnancy (such as going past your due date, or the risk of a medical condition you might have developed in pregnancy).
Risks: The risk of each method of inducing your labour is outlined above. These need to be weighed against the risks to you and to your baby in waiting for labour to start naturally.
Remember:
- Induction may not work.
- There may be a need for an assisted vaginal birth i.e., forceps or ventouse (a suction cap applied to the baby’s head) with the associated increase risk of third or fourth degree tear.
- An induced labour may be more painful than a spontaneous labour.
- There is a chance of over stimulating the uterus.
- If baby’s head is not engaged (well down in your pelvis) when your waters break, there is a small chance of the cord coming out in front of baby’s head (cord prolapse).
- Your place of birth may change from your original plan. This is because we often need to monitor your baby more closely.
Alternatives: You can choose to request a caesarean birth instead of induction, or at any point. You can also delay your induction.
Intuition: What does your intuition say you should do?
Nothing: You can change your mind at any time, or wait a few days to make a decision. If you choose not to have your labour induced, or you choose to wait, you and your baby will be offered regular checks. See 'What happens if I do not choose to have my labour induced?' section.
Second opinion: Do you feel you need to have a conversation with another Midwife or Doctor to help you make your decision.
Induction for concerns with you or your baby
If you choose not to have your labour induced or delay your decision to be induced, the Doctor will put an individual plan in place, including an offer to monitor you and your baby’s wellbeing, this will be discussed and agreed with you.
Continuing pregnancy for more than 41 weeks
If you decide to continue your pregnancy more than 1 week after your estimated due date it is important to be aware of your baby’s movements and contact Maternity Triage if you have any concerns about you or your baby or if you change your mind and wish to have your labour induced.
You will be offered increased monitoring from 42 weeks, which may include:
- Twice weekly checks of your baby’s heartbeat using a CTG monitor.
- Twice weekly ultrasound scans to check the depth of the amniotic fluid (or waters) surrounding your baby and the blood flow through the placenta.
Monitoring only gives information on how your baby is at that moment.
Scans and heartbeat checks cannot reliably predict any changes after the monitoring ends. Adverse effects on the baby (including stillbirth) cannot be predicted or prevented with monitoring.
You can change your mind at any time. Contact your Midwife if you would like to discuss having your labour induced, or as soon as possible if you have any concerns about your baby (for example, reduced or altered fetal movements).
If you require any more information or you have questions at any time during the Induction process, please do not hesitate to ask a Midwife.
If you require any more information or you have questions at any time during the Induction process, please do not hesitate to ask a Midwife.
Contact Numbers:
Labour Ward: 01270 612146
Triage: 01270 273116
Useful web addresses:
National Institute for Health and Care Excellence: Overview | Inducing labour | Guidance | NICE
Tommy's: Inducing Labour
Royal College of Obstetrician and Gynaecologists: Induction of labour information
