 You have just been told that you are having more than one baby. The prospect of a multiple pregnancy can be daunting for even the best intentioned families and we want to ensure that you are fully informed about all aspects of your care.
You have just been told that you are having more than one baby. The prospect of a multiple pregnancy can be daunting for even the best intentioned families and we want to ensure that you are fully informed about all aspects of your care.
For more information about multiple pregnancies please visit: https:/
All naturally conceived pregnancies start in the same way:
- The mother produces an egg, which is released into the fallopian tubes.
- One of the father’s sperm fertilises the egg.
- The fertilised egg develops into an embryo.
With a multiple pregnancy a single egg is fertilised which divides into two, or two separate eggs are fertilised by two separate sperm.
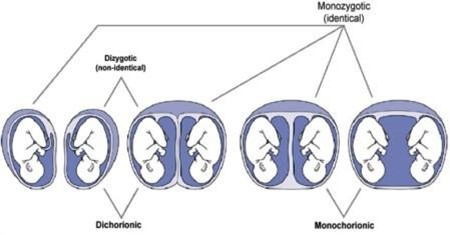
Identical twins are also known as monozygotic because they come from a single fertilised egg which divides. The two babies will be the same sex and share the same genes. Non identical twins are known as dizygotic or fraternal. They come from two separate eggs being fertilised by two separate sperm. Non identical twins are genetically no more alike than any other single born brothers and sisters and they can be either the same sex or a boy and a girl.
Triplets and higher multiples are formed in a similar way, but a combination of these events may occur e.g. resulting in a set of triplets where two are identical and one is not.
At around 12 weeks of pregnancy it is possible to determine whether the babies appear to be identical (monozygotic) or nonidentical (dizygotic or fraternal). A scan will be arranged to look at whether your twins have one or two placentas, this is called establishing chorionicity.
If the babies appear to share the same placenta then the likelihood is that the babies are identical. If the babies do not share a placenta then it is likely they are not identical but a small chance that they are. If at a later stage you find out the sex of the babies and they are different sex, then it is certain they are not identical, but if they are the same sex there is a small chance they are identical.
Here are some terms you may see written in your notes:
DCDA (Di-chorionic Di-amniotic) means that your twins each have their own placenta and are in their own amniotic sac. The majority if these twins are non-identical.
MCDA (Mono-chorionic Di-amniotic) means that your twins are sharing a placenta but are in their own amniotic sac. All of these twins are identical.
MCMA (Mono-chorionic Mono- amniotic) means that your twins are sharing both the placenta and are in the same amniotic sac. All of these twins are identical.
Generally, in a multiple pregnancy you are offered the same tests as a singleton pregnancy and these are explained fully in Screening tests for you and your baby. There are however some exceptions such as screening tests for Down’s, Edwards’ and Patau’s syndromes.
The screening process is different in multiple pregnancies to that of singleton pregnancies. Choosing whether to have the tests is an important decision for you and your babies. You need to make the decision that is right for you.
A screening test is a test offered to all women that carry no risk of miscarriage. For twins the test that you will be offered is called ‘first trimester screening’ or the ‘combined test’ and is a combination of both a blood test and a scan around 12 weeks. This test looks at an area of fluid at the back of each baby’s neck
called the nuchal translucency (NT) to estimate the chance of either baby having Down’s, Edwards’ or Patau’s syndrome. For triplets you will be offered a nuchal translucency scan alone as the additional blood test cannot be done if there are three or more babies. The Midwife or Obstetrician will give you more information about the accuracy of these tests.
If screening in early pregnancy is missed or declined an alternative blood test can be carried out between 14 weeks and 2 days and 20 weeks. For monochorionic twins the detection rate is 80% for a screen positive rate of 3%. For dichorionic twins the detection rate of 40-50% for a screen positive rate of 3%.
If you decide this is something you would like, please speak to your Midwife or Obstetrician.
How common is Down’s syndrome in a multiple pregnancy?
Around 2% of pregnancies affected by Down’s syndrome are twins.
The chance of having a baby with Down’s syndrome is the same in twin pregnancies as it is in singletons. In none identical twins either baby could be affected whereas, if you have identical twins it is most likely that both babies would be affected as they share that same genes.
You will be seen at the hospital regularly during your pregnancy. A pathway of care will be given to you outlining your routine care.
The frequency of your visits to the clinic depends upon:
- The number of babies you are having (twins, triplets or more).
- The type of twin pregnancy (monochorionic or dichorionic).
- Complications which may arise (see next section).
How often will I have ultrasound scans during my pregnancy?
Once it has been decided whether your twins have one or more placentas, further appointments will be made for scans throughout your pregnancy. Dichorionic twins (two separate placentas) are scanned every four weeks from 20 weeks and Monochorionic twins (shared single placenta) are scanned every two weeks from 16 weeks. If you are expecting more than two babies we will discuss your plan of care with you individually.
For more information about your appointments during pregnancy see the following pathways depending which type of multiple pregnancy you have:
What are the common complications of a multiple pregnancy?
Please be reassured that most mums have healthy multiple pregnancies without any problems. However, because you are pregnant with more than one baby you are at a higher risk of maybe developing some complications.
Because of this both you and your babies will be closely monitored as your pregnancy progresses. Many of the complications can only be picked up through scans / urine tests / blood pressure tests, so it is important that you regularly attend your appointments.
What are the risks for the mother?
Vaginal bleeding
This is common early in pregnancy and some women may experience irregular ‘spotting’ throughout their pregnancy without any harm to their babies. However, advice should be sought from a Midwife or your GP with any vaginal bleeding in case of more serious complications.
Anaemia
Anaemia is a common condition in pregnancy but more so in multiple pregnancies. You will be offered blood tests at your first appointment, 24 and 28 weeks to check your iron levels. Symptoms of anaemia include tiredness, light-headedness, looking pale and shortness of breath. If untreated, anaemia can affect the babies’ growth and may increase your risk of complications during pregnancy and after the birth. It is important that you have a diet rich in iron. Because of iron and/or folic acid deficiency, supplements may be prescribed. For more information about anaemia and dietary advice please visit: www.
Gestational hypertension and pre-eclampsia
Gestational hypertension is the term used for high blood pressure that develops in pregnancy. Around 20% of mums carrying multiples will develop high blood pressure. If it progresses with an increase in blood pressure and protein is present in your urine (proteinurea), it is called pre-eclampsia.
This typically happens in the 2nd part of a pregnancy. Other symptoms include nausea and vomiting, upper abdominal pain (epigastric), swelling of the face, hands and ankles, severe headache and disturbed vision. If you do experience any symptoms you must contact Maternity Triage (01270 273116) or your local labour ward (01270 612144) immediately.
If you have one or more of the following risk factors, aspirin will be prescribed from 12 weeks to reduce the likelihood of pre-eclampsia developing:
- This is your first pregnancy.
- You are aged 40 or older.
- Your last pregnancy was more than 10 years ago.
- You are overweight – your BMI (Body Mass Index) is over 30.
- You have a family history of pre-eclampsia.
If pre-eclampsia does develop, admission to hospital may be necessary and medication given to lower your blood pressure. In severe cases of pre-eclampsia it may be necessary for your babies to be born earlier than planned.
Gestational diabetes
This is a condition when your blood glucose (sugar) is raised during pregnancy. It is more likely to occur if you are overweight, have a family history of diabetes or a expecting multiple babies. A further test, called a glucose tolerance test will be done if gestational diabetes is suspected.
If left untreated high blood sugars cause the babies to grow large, increasing the risk of difficult labour, assisted births and caesareans sections. But as twins or multiple babies are usually smaller than singletons this is unlikely to become a problem.
Management of gestational diabetes involves changes to your diet with close monitoring of your blood sugars. If blood sugars do not lower, then medication may be required. Gestational diabetes usually disappears after birth. However, it may re-occur in a future pregnancy or you may develop diabetes at some point later in life. Your GP will discuss this with you at your postnatal appointment.
Postpartum haemorrhage (PPH)
This is severe bleeding after birth and is more common following a multiple birth and after, regardless of the type of birth. This is caused by a failure of the muscles or the womb to contract normally following birth due to their over distension during pregnancy and a larger placenta. For this reason you will be offered an active 3rd stage of labour which means giving you a hormone drug, usually through
a drip which will help your uterus to contract more efficiently and lower the risk of heavy bleeding.
Postnatal depression (PND)
Postnatal depression is a severe form of depression following childbirth that is five times more common in mothers of multiples than mothers of singletons. Caring for multiple babies is more difficult (emotionally, physically and financially) and demanding than caring for one child. It is not uncommon to confuse ‘baby blues’ and PND. Baby blues is a hormonal and physical condition that occurs within the first week or so after childbirth and lasts a few days or weeks. PND can begin as baby blues and last weeks or up to two years. It can be treated if recognised. However, it is important that mums (and dads) seek help if they are concerned they or their partner may be suffering with PND. For more information please visit the Perinatal Mental Health Service page.
What are the risks to babies?
Restricted growth
Because they have to share the same amount of space and nutrition from you, multiple babiess tend to have a lower birth weight than singleton babies of the same gestational age. There may also be discrepancies in weight between the babies because the nutrition that is provided by the placenta is not shared equally. Preterm birth is sometimes recommended if one or more babies are very small or stopped growing.
Twin to Twin Transfusion Syndrome (TTTS) and other complications of sharing a placenta in monochorionic twins
Please see separate leaflet called ‘Monochorionic Twins Complications of Shared Placenta’.
For information about eating healthily, foods to avoid and supplements during pregnancy please visit: Maintaining a healthy pregnancy page.
It is perfectly possible to breastfeed two, three and even four babies. For the mother it can be a very rewarding experience, and for the babies, there is no disputing that breastmilk is the ideal food, and especially so for premature and low birth weight babies who are more susceptible to infections and less able to digest formula milk.
Almost all new mothers who are breastfeeding need some practical help, advice and reassurance, so it is important not to feel you are failing if any problems occur. One of the most common anxieties is that the supply of breastmilk is inadequate. This is rarely true. Almost all mothers have the ability to produce enough milk for twins. The more the baby sucks the more the breasts are stimulated and the more milk is produced. It is a case of supply meets demand.
Correct positioning and attaching of the babies is vital to successful breastfeeding, and without it is one of the main causes of nipple soreness. It is important to seek help from the professionals in the first few days to ensure the babies are positioned correctly and that position is maintained. One baby may be easier to attach than the other, the more difficult baby should be positioned first, then the second baby attached. This often easier if you have someone to help. Feeding the babies simultaneously or individually is a matter of personal choice, it should be whatever suits the mother and her babies best. Until breastfeeding is established, it may be a good idea to swap breasts at each feed to enable both breasts to be stimulated equally.
It is not unusual for twins and multiple births to be born a few weeks early and sometimes may require admission to Special Care Baby Unit. However, many twins are born at around 37 weeks with absolutely no problems. Generally, the sooner the mother has skin to skin contact with her babies and puts them to the breast after birth the better.
If babies are slightly small they may need some assistance with feeding initially. This may require giving expressed breastmilk either by a tube into the babies stomach or via a cup. Even very small babies can take milk via a cup, a midwife or neonatal nurse would be able to demonstrate and advise.
It is important for all breastfeeding mothers to get sufficient rest, have a well balanced diet, and an adequate fluid intake. However, it is especially necessary for mothers of twins. All sensible offers of help should be gratefully accepted, and mothers should ensure they have three substantial meals, plus extra snacks and drinks on hand whilst actually feeding.
If the supply of breastmilk is insufficient, it is better to introduce one or two bottles and combine breast and bottle feeds rather than give up breast feeding completely. Even a small amount of breast milk each day for a short period of time is better than none at all.
Triplets and quadruplets are more likely to be born several weeks early and are more likely to be admitted to Special Care Baby Unit. If well enough they should be encouraged to nuzzle at the breast. However, until they are able to suck, their feeds will need to be given via a tube. Breastmilk can be expressed to stimulate milk production and breast and formula feeds combined to ensure all babies have their quota of breastmilk.
For more information please visit the Feeding your baby page.
Financial Benefits
There are no additional maternal or paternal financial benefits for parents of twin or multiple pregnancies during the antenatal period. The entitlements for maternity pay and paternity pay vary according to circumstance and employer but remain the same for both single and multiple pregnancies.
There are a number of different benefits and tax credits you may be entitled to. Contact your local Citizens Advice or visit www.
Maternity leave
Statutory Maternity leave extends for 52 weeks regardless of length of service, hours worked and amount of pay, plus any additional from employers own scheme, and regardless of single or multiple pregnancy. Your employer should be informed by 15th week before the EDD (expected date of delivery) of your EDD and the date you are expected to start maternity leave. Your midwife will give you a MAT B1 form which confirms your EDD and you can give this to your employer. For more information please visit: www.
Twins are at slightly higher risk of problems around the time of labour and birth as compared to single babies. When a twin pregnancy is at term (37 weeks or more) and the first twin is in the head down position, a decision needs to be made as to whether the babies would be best born by vaginal birth, or whether a caesarean birth should be undertaken. With triplets or more, caesarean birth is advised.
Place and timing of birth
All multiple pregnancies are advised to birth in hospital because there is a higher chance of complications with multiple births.
You may need to move your care to another hospital with appropriate facilities if complications in your pregnancy indicate an early birth: this may not be near to home if you want to try and ensure there are enough beds for both your babies in the Neonatal Unit.
If your pregnancy has been without complications, you will be offered an elective birth (either by induction or caesarean birth) from the following times depending on your pregnancy:
- At 37 weeks if you are carrying dichorionic twins.
- At 36 weeks if you are carrying monochorionic/diamniotic twins.
- Between 32+0 and 33+6 weeks for monochorionic monoamniotic twins.
- At 35 weeks if you are carrying triplets.
Having an elective birth at these times is not thought to increase the risk of health problems for your babies. You can choose not to have an elective birth at the times recommended here; however, continuing your pregnancy for longer may increase your risk of complications, including stillbirth.
Your doctor or midwife will explain all the risks and benefits of the possible options when planning the birth of your babies. You will be offered a tour of the Neonatal Unit so you know what to expect if your babies are born early or need additional care.
If you are having an elective birth for triplets at 35 weeks or for monochorionic twins at 36 weeks, you should be offered a course of steroids (usually given by injection) before your birth. Steroids help to mature the lungs of premature babies, and reduce breathing problems after they are born. You should only be offered steroids if birth is planned or likely to happen soon: it is not thought helpful to have one or more courses of steroids before birth is imminent.
If you choose not to have an elective birth at the times recommended on the previous page, you will need to be monitored regularly to check that you and your babies remain healthy. You should be offered weekly appointments with an obstetrician and should have a scan at each appointment (the babies’ growth will be measured every two weeks on the scan).
What happens if I go into labour before that decision is made?
60% of multiple pregnancies result in spontaneous birth before 37 weeks. A full assessment will be made by the midwife and obstetrician on admission to the labour ward and an appropriate and safe plan for birth will be discussed with you. An ultrasound scan will be performed on admission to see which way your babies are lying that will help to inform the decision.
What are the risks of giving birth to twins?
Although problems may occur during any labour or vaginal birth, there is some evidence that twin pregnancies near term have higher rates of complications than pregnancies with only one baby. These complications might arise because of problems during pregnancy, or labour and birth.
Both twins may be at risk but birth complications more often happen for the second twin after the birth of the first twin.
If you are pregnant with twins, there is now evidence suggesting there is no increased risk to your babies whether they are born by caesarean birth or vaginal birth. In the UK almost half of all twins are born vaginally.
Three clinical trials have shown that a planned caesarean birth compared with a planned vaginal birth was associated with a small increase in short-term serious maternal health issues.
Caesarean birth is also associated with a higher risk of blood clots in the legs or lungs, an increased length of stay in hospital and increased pain with restrictions on driving for several weeks following the procedure.
We also know that there are serious long- term risks of caesarean birth for the mother. These include problems with future pregnancies, such as uterine scar rupture, increased risk of repeat caesarean birth (44% in a UK study) and problems with the placenta in future pregnancies. However, we do not yet have enough information to say how big these risks are.
Caesarean is also associated with an increased risk of the babies having respiratory distress after birth.
As we have said, there is no evidence to justify either routine caesarean birth or routine vaginal birth . As there are recognised hazards of caesarean birth to the mother, but no evidence to prove any benefit to the baby from caesarean birth, a vaginal birth is recommended if the leading twin is head down. The risk of serious problems for the baby are low (less than 5 in 1000 having a significant problem at the time of the birth). However 30% of women who choose a vaginal birth will end up having a caesarean birth.
Even if the first twin is head down you may be advised to have a caesarean for other reasons eg. low placenta, previous caesarean.
In very rare cases, you may give birth to one twin vaginally and then require a caesarean birth for the second twin if the baby becomes distressed. This occurs in less than 5% of twin births.
If you are pregnant with more than two babies your obstetrician will discuss with you the safest route of birth. They are likely to recommend caesarean birth.
In the third trimester, usually by 32 weeks gestation when the babies have settled into position, you will have the opportunity to discuss the pros and cons of vaginal birth versus caesarean and come to an informed decision about how you want to give birth to your babies.
Care during labour
The process of labour is the same, but the babies will be closely monitored. You will be given a drip in case it is needed later.
During labour and at the time of birth, there will be additional midwives and doctors caring for you than there may have been if there were only one baby. At times it will probably be necessary for a number of those staff and extra equipment to be present in the room with you.
Monitoring your babies during labour and birth
We recommend that your babies’ heart rates are monitored continuously throughout your labour and birth. This is particularly important for the second twin as it is the baby most at risk. To do this, an electronic monitor will be used and a clip might be applied to the first baby’s head once your waters have broken.
Pain relief in labour
In the antenatal period you will have the opportunity to discuss all methods of pain relief available during labour.
There is a risk that after birth of the first twin that twin two could move into an awkward position. This is particularly possible if the second twin is not head down at the end of pregnancy (i.e. is breech or transverse) but can also happen if it is head down. This requires assistance and potentially painful procedures to be performed as a matter of urgency in order for your baby to be born safely. It is therefore recommended that all women in labour with twins have adequate pain relief for time of birth. This would assist emergency procedures should there be any risk of distress in twin two. For this reason you may be advised to have an epidural.
An epidural may also be recommended if there are antenatal complications such as raised blood pressure.
It is ultimately a personal decision which type of pain relief you choose but you will have the opportunity to discuss this further.
What happens if I need an emergency caesarean birth?
The Labour Ward is equipped with a fully operational theatre therefore any emergency surgery can be done without moving to another part of the hospital.
What happens if I go into labour prematurely?
A full term pregnancy takes about 40 weeks to complete. Babies born before 37 weeks may have problems breathing, eating and keeping warm and are more prone to jaundice. The earlier a baby is born the more the risk.
Premature labour is when labour occurs between the 24th and 37th week of pregnancy, when uterine contractions cause the cervix, the mouth of the uterus or womb, to open earlier than normal. This can result in premature birth.
Certain factors may increase a woman’s chances of having premature labour, such as carrying twins or triplets. About 55-60% of twins and 75% of triplets are born early i.e. before 37 weeks. However, the specific cause or causes of premature labour are not known. Sometimes
a woman may have premature labour for no apparent reason.
Warning signs of premature labour
It may be possible to prevent a premature birth by knowing the warning signs of premature labour and by seeking care early if these signs occur. Warning signs and symptoms for premature labour include:
Uterine contractions that happen six or more times in an hour, with or without any other warning signs.
- Menstrual-like cramps felt in the lower abdomen that may come and go or be constant.
- Low dull backache felt below the waistline that may come and go or be constant.
- Pelvic pressure that feels like your baby is pushing down. This pressure comes and goes.
- Abdominal cramping with or without diarrhoea.
- Increase or change in vaginal discharge such as change into a mucousy, watery or bloody discharge.
For more information about preterm labour please visit the Preterm birth page.
Uterine contractions: how to tell what is normal
It is normal to have some uterine contractions throughout the day. They often occur when you change positions, such as from sitting to lying down. It is not normal to have frequent uterine contractions, such as six or more in one hour. Frequent uterine contractions or tightenings may cause your cervix to begin to open.
Since the onset of premature labour is very subtle and often hard to recognize, it is important to know how to feel your abdomen for uterine contractions. You can feel for contractions in this way:
- While lying down, place your fingertips on the top of your uterus
- A contraction is a periodic tightening or hardening of your uterus. If your uterus is contracting, you will actually feel your abdomen get tight or hard, and then feel it relax or soften when the contraction is over.
What to do if you think you may have symptoms of premature labour
If you think you are having uterine contractions or any other signs and symptoms of premature labour:
- Lie down tilted towards your side. Place a pillow at your back for support.
- Sometimes lying down for an hour may slow down or stop the signs and symptoms.
- Do not lie flat on your back, because lying flat may cause the contractions to occur more often.
- Do not turn completely on your side, because you may not be able to feel the contractions.
- Hydrate yourself by drinking several large glasses of water. Sometimes being dehydrated can cause contractions.
- Check for contractions for one hour.
- To tell how often contractions are occurring, check the minutes that elapse from the beginning of one contraction to the beginning of the next.
Call the hospital or go to the hospital if you experience any of the following:
- Have six or more uterine contractions in one hour.
- Have any of the other signs and symptoms for one hour.
- Have any spotting or leaking of fluid from your vagina.
If it is likely that your babies are going to be born prematurely, you will need to be admitted to hospital and assessed so that your condition and the condition of the babies can be monitored closely. You may be given treatment to delay the labour, and treated with steroid injections to help mature the babies’ lungs. The babies are likely to be admitted to the Neonatal Unit as they may need help with feeding or breathing. If there is time before the birth of your babies, the midwife will arrange for you to speak to a paediatrician and staff from the Neonatal Unit. If the labour happens before 27 weeks gestation, you will be assessed on the Labour Ward by an obstetrician and transferred to a Regional Neonatal Centre with services designed for very premature babies.
The Neonatal Unit offers three different levels of care. These are:
Intensive Care: This is the highest level of care and babies may be nursed one to one. Processes that fall into this category include types of respiratory support and intravenous feeding.
High Dependency: This care may include some respiratory support and some intravenous feeding. Though babies will be monitored they will not require one to one nursing.
Special Care: These babies require a low level of support which can include tube feeding, oxygen or phototherapy.
Babies who have needed a higher level of care but are now recovering will move onto this level of care as they continue to improve before discharge home.
Will our babies automatically be admitted to the Neonatal Unit?
The simple answer is no but if your babies are born before 35 weeks then they are likely to initially be cared for on the Neonatal Unit. In just under half of twins at least one of the babies spends time in neonatal care, while over 90% of triplets require neonatal care.
Will they be separated?
Your babies may need to be nursed separately but this depends on the reason foradmission. Whilst every effort will be made to keep your babies in the same room, this cannot be guaranteed.
The babies will always be treated as individuals and this may mean that if they require different levels of care they may be in different rooms. Once your babies are well enough to be cared for in a normal cot it should be possible for them to be put together in one cot.
Quite often babies will be ready for discharge at the same time but this is not always the case. Sometimes it may be appropriate to discharge your babies at different times. When this occurs it is possible to bring the baby back to the unit when you are visiting.
Will we be able to visit and stay with our babies?
We use a family centred approach in the care we give to the babies on the unit. This means that we actively encourage parents to get involved in decisions about the care their babies receive and the giving of that care.
Support and teaching will be given so that you can get involved in your babies care. Even if your baby is receiving intensive care it may be possible for you to change their nappy or give ‘containment holding’ which is a kind of ‘cuddle in an incubator’. This sort of physical contact can be very reassuring for a baby and minimise discomfort and stress for them.
We understand that family circumstances may vary, so please discuss with staff if these guidelines do not suit your family. We may be able to arrange changes for you.
Is it possible to breast feed twins or more if they go to special care?
The simple answer is yes. We have had families who have had multiple births who have gone home breast-feeding successfully. In some of these cases the babies had been very early or very poorly. If your babies are born early or are poorly they may not be able to go to the breast immediately. In these circumstances you will be given support and advice to start your milk supply and maintain it by expressing until your babies are ready to feed. We will be able to supply you with all the equipment that you need.
As well as all the information and skills that any breast feeding mum would need, lots of help and support will be given to show you how you can feed two babies at the same time. Breast milk is best for all babies but for those born small, early or poorly it is even more important. Even if you are planning to bottle feed in the long term it will be of great benefit to them if you express your milk for them initially.
With this in mind we have a human supplement supply until you are able to meet your babies needs yourself. It can also be used for babies whose mums are unable to express. All the donor mums undergo an in- depth screening programme before they start donating and all milk is screened before and after pasteurisation. Staff will explain this to you fully should the need arise.
As soon as your babies are born, identification bands will be attached to your babies’ ankles. It does not matter if you have not chosen names as twin one and twin two will be written on initially. If all is well and your babies can do skin to skin/early first feed, they will be transferred with you to the postnatal ward.
Once on the postnatal ward your babies will be kept with you at all times and may share one cot or be nursed separately. The staff on the ward will help and support you and your babies during your stay.
If you need help with feeding or caring for your babies, please ask.
How long will we need to stay in hospital?
The length of your hospital stay will depend on the type of birth and the age of the babies when born. If all is well your stay may only be 24-48 hours. It is important to fully prepare for the discharge home to ensure you have everything you need to care for yourself and your babies.
Think about how you can use your space at home creatively to make life easier e.g. sleeping arrangements, feeding and washing. Friends and family members are always willing to help. Discuss and plan how they can help with household chores e.g. shopping, washing, cooking etc. It is important that you and your partner have time to spend getting to know your babies together. Remember to ensure you have two or more appropriate car seats to transfer your babies home and you practice fitting them beforehand.
What happens when we are discharged home from the ward?
Your community midwife will be informed of your discharge and will visit you at home the following day when a plan of care will be discussed. The early days at home with your babies can be very tiring and you may find it useful to limit visits by friends and neighbours. Remember to make time to look after yourselves as well as your babies.
What support is available in the community?
The health visitor will visit you at home by appointment, usually between the 10th and 14th day after discharge. She will discuss how best she can support you and your babies in the early weeks and will give you information about how to access advice and support locally.
There are several twins and triplet multiples groups in the area. You may find it useful to visit a group during your pregnancy to meet other families with multiples to help prepare you and your family. You may find it useful to access the Twins Trust website for more information.
What happens if my babies need to stay on the Neonatal Unit and I am discharged home?
If one or more of your babies are on the Neonatal Unit, you may be discharged home from the ward. The neonatal staff will support you to come into the unit daily to help care for your babies (Please also see the neonatal section).
